Diabetes mellitus refers to a group of conditions that impact the body’s ability to regulate blood sugar (glucose). Glucose is a key source of energy for muscles, tissues, and the brain.
The cause of diabetes varies depending on the type. Regardless of the type, diabetes leads to elevated sugar levels in the blood, which can cause serious health complications.
Chronic diabetes conditions include type 1 and type 2 diabetes.
Prediabetes and gestational diabetes are reversible conditions. Prediabetes occurs when blood sugar levels are higher than normal but not yet high enough to be classified as diabetes. Without intervention, prediabetes can progress to diabetes. Gestational diabetes happens during pregnancy and typically resolves after childbirth.
Symptoms
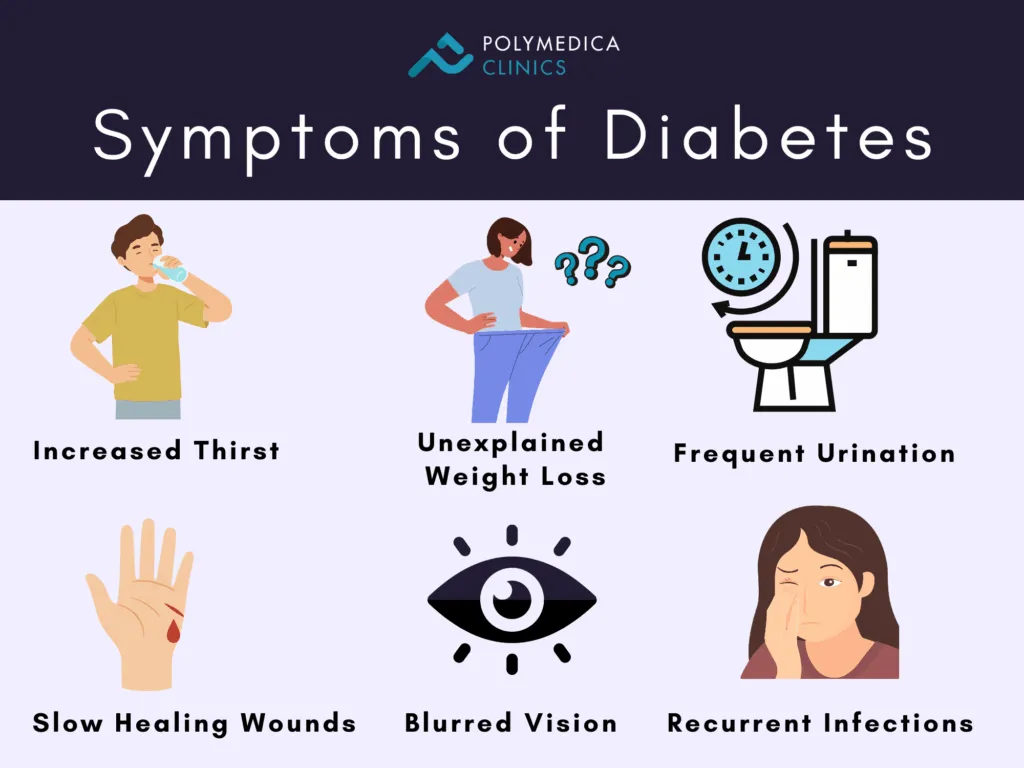
The symptoms of diabetes depend on how high blood sugar levels are. Some individuals, particularly those with prediabetes, gestational diabetes, or type 2 diabetes, may not experience any noticeable symptoms. Type 1 diabetes often presents symptoms quickly and can be more severe.
Some common symptoms of both type 1 and type 2 diabetes include:
Increased thirst
Frequent urination
Unexplained weight loss
Fatigue and weakness
Irritability and other mood changes
Blurred vision
Slow-healing sores
Recurrent infections, such as gum, skin, and vaginal infections
Presence of ketones in the urine, which are produced when the body lacks sufficient insulin
Type 1 diabetes typically begins in childhood or adolescence, while type 2 diabetes, which is more common, can develop at any age. It is more frequent in individuals over 40, but the incidence of type 2 diabetes in children is rising.
When to Visit an Endocrinologist
If there are any signs or symptoms of diabetes, it is essential to consult an endocrinologist. Early detection allows for prompt treatment. For those who have already been diagnosed, regular follow-up care is necessary to manage blood sugar levels effectively.
Causes
Understanding how the body uses glucose is key to understanding diabetes.
How Insulin Functions
Insulin is a hormone produced by the pancreas, an organ located behind and beneath the stomach. The pancreas releases insulin into the bloodstream. Insulin allows glucose to enter cells, lowering blood sugar levels. As blood sugar drops, the pancreas reduces the secretion of insulin.
The Role of Glucose
Glucose, a type of sugar, is essential for energy production in the body. It comes from two main sources: food and the liver. After food is consumed, glucose enters the bloodstream and is absorbed by cells with the help of insulin. The liver both stores and produces glucose. When glucose levels drop, such as between meals, the liver breaks down stored glycogen into glucose to maintain normal levels in the blood.
The exact cause of most types of diabetes remains unclear. However, in all cases, insulin does not work properly, which is either due to its decreased secretion, which is what happens in type 1 diabetes. Or due to insulin resistance, which occurs in other types. Both type 1 and type 2 diabetes are believed to be influenced by a combination of genetic and environmental factors, although these remain uncertain.
Risk Factors
The risk factors for diabetes vary depending on the type. A family history of diabetes can play a role in all types. Environmental factors, as well as geographic location, can increase the risk of type 1 diabetes. Family members of those with type 1 diabetes may be tested for autoimmune markers (autoantibodies), which indicate an increased risk of developing type 1 diabetes. However, not everyone with these markers develops the disease.
Being overweight or obese significantly raises the likelihood of developing prediabetes, type 2 diabetes, and gestational diabetes.
Complications
The long-term complications of diabetes develop gradually. The longer diabetes goes untreated or is poorly managed, the higher the risk of complications, which can be disabling or even life-threatening. In fact, prediabetes can progress into type 2 diabetes. Some potential complications include:
Cardiovascular Disease: Diabetes greatly increases the risk of heart disease, stroke, and narrowing of arteries.
Neuropathy: High blood sugar can damage the small blood vessels that nourish nerves, especially in the legs, causing tingling, numbness, and pain.
Kidney Damage: The kidneys’ filtering system can be damaged by diabetes, leading to kidney disease.
Retinopathy: Diabetes can damage the blood vessels in the eyes, potentially causing blindness.
Foot Problems: Nerve damage and poor blood circulation in the feet increase the risk of foot complications.
Skin and Oral Issues: Diabetic individuals may be more prone to infections, including bacterial and fungal infections.
Hearing Loss: Hearing problems are more common in people with diabetes.
Alzheimer’s Disease: Type 2 diabetes may increase the risk of cognitive decline and dementia.
Depression: Individuals with both type 1 and type 2 diabetes may experience higher rates of depression.
Complications of Gestational Diabetes
Although most women with gestational diabetes deliver healthy babies, uncontrolled blood sugar can cause problems. Potential complications for the baby may include:
Excess Growth: Extra glucose can cross the placenta, leading to the baby’s pancreas producing more insulin, which can result in an abnormally large baby and may require a caesarean section.
Hypoglycemia: Babies may develop low blood sugar after birth due to the excess insulin produced during pregnancy.
Increased Risk of Type 2 Diabetes: Children born to mothers with gestational diabetes have a higher risk of obesity and type 2 diabetes later in life.
Fetal Death: Untreated gestational diabetes can lead to fetal death, either before or shortly after birth.
Mothers may also experience complications, including:
Preeclampsia: Characterized by high blood pressure, protein in the urine, and swelling in the legs and feet.
Recurrence of Gestational Diabetes: Women who had gestational diabetes in one pregnancy are more likely to experience it again in future pregnancies.
Prevention
While type 1 diabetes cannot be prevented, adopting healthy lifestyle choices can help reduce the risk of developing prediabetes, type 2 diabetes, and gestational diabetes.
Eat a Healthy Diet: Focus on low-fat, low-calorie foods that are high in fiber. Include a variety of fruits, vegetables, and whole grains in the diet.
Increase Physical Activity: Aim for 30 minutes of moderate aerobic activity most days of the week, or at least 150 minutes of exercise per week. Brisk walking is an excellent way to meet this goal.
Lose Excess Weight: Even a 7% reduction in body weight can lower the risk of diabetes. For example, losing about 6.4 kilograms for someone weighing 90.7 kilograms can reduce the likelihood of developing diabetes. Weight loss should not be pursued during pregnancy. Consult with your doctor to determine a healthy weight gain during pregnancy. In some cases, medications like metformin may be prescribed to help lower the risk of type 2 diabetes. However, lifestyle changes remain the most important strategy. Individuals with prediabetes should have their blood sugar levels checked at least annually to monitor for potential progression to type 2 diabetes.
Testing Overview
Type 1 diabetes often presents with sudden symptoms, making blood sugar testing necessary. Unlike other types of diabetes and prediabetes, which develop gradually and may not show clear symptoms, the American Diabetes Association (ADA) has established guidelines for screening. These guidelines suggest screening for the following groups:
Individuals with a body mass index (BMI) over 25 and additional risk factors such as high blood pressure, abnormal cholesterol levels, a sedentary lifestyle, a history of polycystic ovary syndrome or heart disease, or a family history of diabetes.
Individuals over 35 years of age should undergo an initial blood sugar test, with follow-up tests every three years if results are normal.
Women who have previously had gestational diabetes should be screened every three years.
Those diagnosed with prediabetes should undergo annual testing.
Treatment Overview
Managing diabetes typically involves blood sugar monitoring, insulin, or oral medication, alongside a healthy diet, weight control, and regular physical activity.
Healthy Eating: A balanced diet focusing on fruits, vegetables, lean proteins, and whole grains is essential for managing blood sugar levels. Reducing saturated fats, refined carbohydrates, and sweets is recommended. A registered dietitian can help develop a personalized meal plan, especially for those using insulin or managing type 1 diabetes, where carbohydrate counting is important.
Physical Activity: Regular aerobic exercise helps regulate blood sugar by increasing insulin sensitivity. Most individuals should aim for at least 30 minutes of moderate activity most days of the week, totaling at least 150 minutes weekly. This can include walking, swimming, or cycling. Gradually building activity levels is advisable for those who have been inactive.
Type 1 and Type 2 Diabetes Treatment
Type 1 Diabetes: Treatment requires insulin injections or an insulin pump, regular blood sugar checks, and carbohydrate counting.
An insulin pump is a small device attached to the body that delivers precise doses of insulin throughout the day, helping to control blood sugar more accurately and reducing the need for frequent injections.Type 2 Diabetes: Treatment primarily involves lifestyle changes, blood sugar monitoring, and possibly oral medications, insulin, or both.
Blood sugar monitoring varies by individual treatment plans. For those on insulin therapy, regular checks are essential, sometimes involving continuous glucose monitoring to track trends without frequent finger pricks.Diabetes Remission:
In some individuals with type 2 diabetes, it is possible to achieve remission, a state where blood glucose levels return to below the diabetes range without the need for medication.
Remission is generally defined as maintaining an HbA1c level of less than 6.5% for at least three months without glucose-lowering drugs. Significant and sustained weight loss, healthy dietary habits, and increased physical activity are key contributors to remission. In certain cases, GLP-1 medications or bariatric (weight loss) surgery have also been shown to produce long-term remission, particularly in individuals with obesity.
However, remission does not mean the disease is cured; continuous monitoring and lifestyle management remain essential to prevent relapse.
Ongoing Management
Regular monitoring of blood sugar, HbA1C levels, and blood pressure is essential for ongoing diabetes management. Even for individuals who achieve remission, periodic testing remains important to ensure blood glucose levels remain within the normal range.
Regular eye exams are necessary to detect any diabetic retinopathy early, while routine dental visits are crucial to prevent gum disease and other complications related to diabetes. Foot care should also be an integral part of monitoring, as individuals with diabetes are at a higher risk for infections and foot problems.
Maintaining a healthy weight, eating a balanced diet, and incorporating physical activity into daily routines are critical to managing blood sugar levels. Avoiding smoking, controlling stress, and staying informed about advancements in diabetes treatments can improve long-term outcomes. Regular physical check-ups with an endocrinologist help ensure that all aspects of diabetes care are addressed.