Hyperlipidemia, commonly known as high cholesterol, is a condition in which there is an excessive amount of fats (lipids) in the blood. These fats travel through your bloodstream so your body can use them for energy and cell functions. However, when levels are too high, they can interfere with normal blood flow through the arteries, increasing the risk of heart attacks and strokes.
Overview
Types of cholesterol and their roles
Lipids are a group of fat‑like substances in your blood that include cholesterol and triglycerides. They are essential for your body to build cells, make hormones, and store energy.
Cholesterol is one type of lipid. Your body makes cholesterol in the liver, and you also get some from food. Cholesterol itself is not bad, but certain types can be harmful when they are too high.
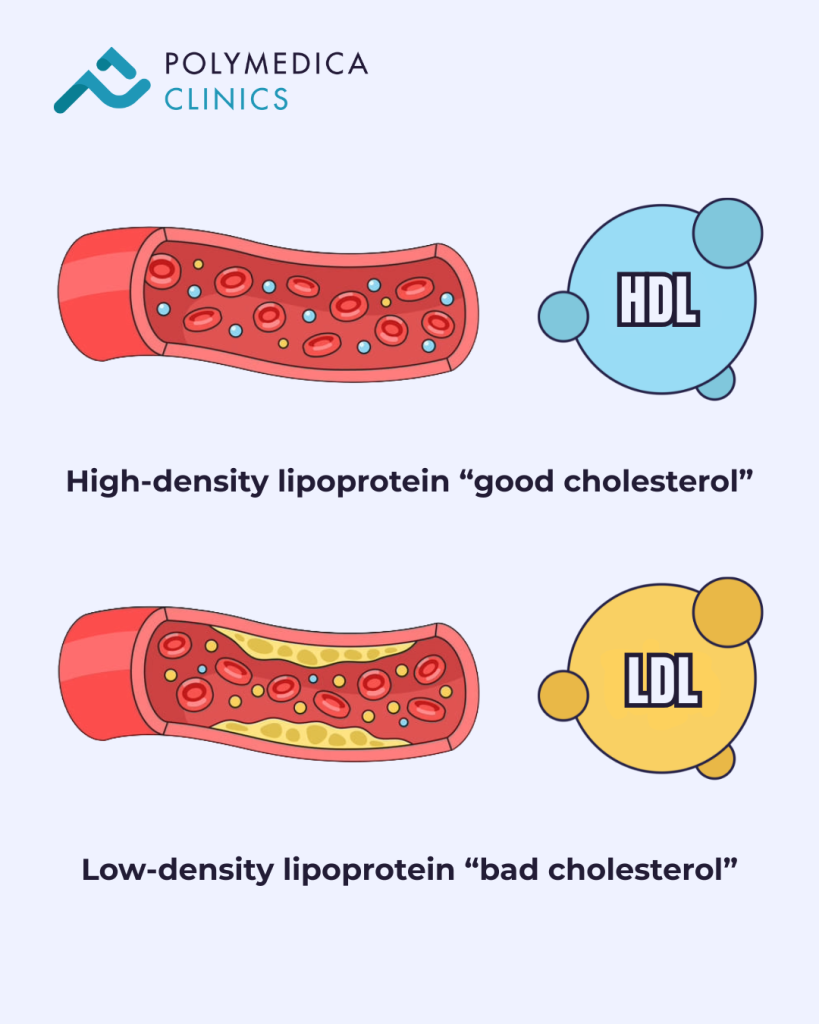
Cholesterol travels in the bloodstream inside carriers called lipoproteins:
High‑density lipoprotein (HDL) is known as “good cholesterol” because it helps remove excess cholesterol from your blood and artery walls and carries it back to the liver for disposal.
Low‑density lipoprotein (LDL) is often called “bad cholesterol” because high levels of LDL can deposit cholesterol in your artery walls, forming plaque. This plaque can narrow or block arteries and increase the risk of heart disease.
Very low-density lipoprotein (VLDL)
Another harmful type, VLDL, carries triglycerides that also contribute to plaque formation.
A cardiologist evaluates cholesterol values together with other cardiovascular risk factors when deciding on treatment.
What is hyperlipidemia?
Hyperlipidemia, also referred to as dyslipidemia, means that lipid levels in the blood are higher than normal. Most of the cholesterol in your blood (about 80 percent) is produced naturally by your liver and body cells. Only about 20 percent comes from the food you eat. Dietary cholesterol alone (for example, in eggs and seafood) is not the main factor causing high blood cholesterol, as was once thought, but rather it is foods that are also high in trans fats or saturated fats that can raise LDL (“bad cholesterol”), lower HDL (“good cholesterol”), and stimulate the liver to produce more cholesterol.
Trans fats are primarily artificial fats made by adding hydrogen to vegetable oils to make them more solid, though small amounts occur naturally in some animal products. Artificial trans fats have been banned in many countries, but some packaged and fried foods may still contain them. In Egypt, trans fats may still be present in processed foods such as biscuits, frosting, fried street foods, and some vegetable shortenings. Always check food labels and totally avoid trans fat content.
Saturated fats occur naturally in foods such as red meats (beef and lamb), poultry with skin, butter, ghee, cream, and cheeses. Not all saturated fats are equally harmful, but high intake increases LDL. Experts recommend limiting daily intake of saturated fats to approximately 13 grams for most people.
Dyslipidemia vs. hyperlipidemia
The terms are often used interchangeably. Dyslipidemia may also describe abnormal cholesterol function, such as an unhealthy balance between LDL and HDL or cholesterol particles that promote inflammation, even when total cholesterol levels are not markedly elevated.
Both elevated cholesterol and abnormal cholesterol behavior increase the risk of cardiovascular disease and require evaluation by a cardiologist.
How common is hyperlipidemia?
Hyperlipidemia is very common worldwide, including in Egypt, where many adults have elevated cholesterol levels, often without noticeable symptoms.
How dangerous is high cholesterol?
If hyperlipidemia is not treated, cholesterol plaque continues to accumulate in the arteries over time. This increases the risk of heart attacks and strokes by reducing blood flow to the heart and brain. Cardiovascular disease remains one of the leading causes of death globally.
Effects of hyperlipidemia on the body
Untreated hyperlipidemia can cause atherosclerosis, leading to complications such as:
- Heart attack
- Stroke
- Coronary artery disease
- Carotid artery disease
- Sudden cardiac arrest
- Peripheral artery disease
- Microvascular disease
Signs and Symptoms
How does high cholesterol feel?
High cholesterol usually causes no symptoms in its early stages. Over time, plaque buildup may restrict blood flow to the heart or brain. Symptoms of coronary artery disease can include chest pain during physical activity, jaw pain, and shortness of breath.
If a plaque ruptures and a blood clot forms, it may completely block an artery, causing a heart attack. Symptoms include severe chest pain, nausea, flushing, and difficulty breathing. This is a medical emergency requiring immediate emergency care.
Are there warning signs?
Most people experience no warning signs. Some individuals with cholesterol disorders may develop xanthomas (fatty deposits under the skin), xanthelasmas (fatty deposits on the eyelids), or corneal arcus (a pale ring around the colored part of the eye). Conditions such as obesity may prompt a cardiologist to assess cholesterol levels.
Causes
What causes cholesterol levels to rise?
Common causes include:
- Smoking
- Diets high in saturated or trans fats
- Physical inactivity
- Chronic stress
- Genetic factors affecting cholesterol metabolism
Certain medications may raise cholesterol levels, including:
- Beta-blockers
- Diuretics
- Hormonal contraceptives
- Steroids
Medical conditions that can affect cholesterol levels include:
- Overweight and obesity
- Liver disease
- Pancreatic disease
- Multiple myeloma
- Polycystic ovary syndrome (PCOS)
- Hypothyroidism
- Primary biliary cholangitis
- Chronic kidney disease
- Diabetes
- Lupus
- Sleep apnea
Risk factors for hyperlipidemia
Risk is higher if you:
- Have a family history of high cholesterol
- Have hypothyroidism
- Are overweight or obese
- Eat an unhealthy diet
- Have diabetes
- Smoke
Diagnosis and Tests
How is hyperlipidemia diagnosed?
A cardiologist typically performs:
- A physical examination
- A review of personal and family medical history
- Blood tests to measure cholesterol levels
The cardiologist may also estimate a patient’s 10-year cardiovascular disease risk using clinical risk assessment tools.
Lipid panel reference values
| Type of Lipid | Recommended Level |
|---|---|
| Total cholesterol | Less than 200 mg/dL |
| LDL (bad cholesterol) | Less than 100 mg/dL |
| HDL (good cholesterol) | 60 mg/dL or higher |
| Triglycerides | Less than 150 mg/dL |
Total cholesterol classification:
- Less than 200 mg/dL – Optimal
- 200–239 mg/dL – Borderline high
- 240 mg/dL or higher – High
Additional diagnostic tests
In selected cases, a cardiologist may request:
- High-sensitivity C-reactive protein (hs-CRP)
- Lipoprotein (a)
- Apolipoprotein B
- Coronary artery calcium scoring
Management and Treatment
How is hyperlipidemia treated?
Some patients can control cholesterol with lifestyle changes alone, while others require medication prescribed by a cardiologist. Management strategies include:
- Regular physical activity
- Smoking cessation
- Sleeping at least seven hours per night
- Stress management
- Eating heart-healthy foods
- Achieving and maintaining a healthy weight
Medications for hyperlipidemia
The most commonly prescribed medications are statins, which reduce LDL cholesterol levels. A cardiologist may prescribe alternative or additional medications if:
- Statins are not tolerated
- Cholesterol targets are not reached
- Familial hypercholesterolemia is present
Side effects of treatment
Cholesterol‑lowering medications, especially statins, can cause side effects such as mild muscle aches, headaches, or digestive discomfort, but serious problems are uncommon. A small percentage of patients may experience a mild elevation of liver enzymes, but large clinical studies show that clinically important liver injury from statins is very rare, occurring at a rate similar to or only slightly above background rates in the general population, and mild elevations in liver enzymes affect only a small percentage of patients. Patients should report any side effects to their cardiologist, who can evaluate them, adjust treatment, or suggest alternatives if necessary. Widespread claims questioning the safety or necessity of statins are not supported by rigorous clinical studies. To the contrary, the evidence clearly shows that the benefits of statins in reducing the risk of heart attacks and strokes generally outweigh their risks for most patients with high LDL cholesterol.
When will treatment start working?
A cardiologist usually repeats cholesterol tests 2–3 months after starting treatment. Cholesterol control is long-term, and many patients require ongoing therapy to reduce cardiovascular risk.
Outlook / Prognosis
What should I expect?
People with hyperlipidemia need to maintain healthy habits long-term and attend regular follow-up visits with their cardiologist. When cholesterol is well controlled, the risk of serious complications is significantly reduced.
How long does hyperlipidemia last?
Hyperlipidemia is a chronic condition that requires lifelong management under cardiology care.
Overall outlook
Although high cholesterol increases the risk of heart disease and stroke, proper treatment and follow-up with a cardiologist greatly improve long-term outcomes.
Prevention
How can I reduce my risk?
Children with a family history of heart disease may benefit from early cholesterol screening. Adults should have regular cholesterol checks, with frequency determined by a cardiologist based on age and risk factors.
How can hyperlipidemia be prevented?
Preventive steps include:
- Quitting smoking
- Staying physically active
- Managing stress effectively
- Getting adequate sleep
- Eating a balanced, nutritious diet
- Completely avoiding trans fats
- Maintaining a healthy body weight
Living With Hyperlipidemia
How do I take care of myself?
Follow your cardiologist’s recommendations closely. Helpful steps include:
- Exercising regularly
- Avoiding tobacco products
- Sleeping at least seven hours per night
- Managing stress
- Eating healthier foods
- Maintaining a healthy weight
Additional measures:
- Take medications exactly as prescribed by your cardiologist
- Discuss your cardiovascular risk regularly
- Keep all scheduled follow-up appointments